Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. The exact cause of PCOS is not fully understood, but it is primarily associated with hormonal imbalances, insulin resistance, and genetics.
It manifests through various symptoms, including irregular menstrual cycles, excessive androgen levels, weight gain, acne, and even infertility. While there is no definitive cure for PCOS, managing its symptoms and improving overall health is possible through lifestyle changes, particularly dietary modifications.
In fact, the right diet can play a crucial role in PCOS treatment, helping to manage symptoms, enhance fertility, and support overall hormonal balance. This article explores the role of diet in PCOS, highlighting foods to eat and avoid, and how specific dietary approaches can benefit those dealing with PCOS.
Understanding PCOS and Its Symptoms
PCOS affects millions of women worldwide and can present a wide array of symptoms, such as:
- Irregular periods or no periods at all
- Excessive hair growth (hirsutism), often on the face, chest, or back
- Acne or oily skin
- Thinning hair or hair loss from the head
- Weight gain, particularly around the abdomen
- Difficulty getting pregnant (due to irregular ovulation or lack of ovulation)
- Insulin resistance and higher risk of developing type 2 diabetes
- Mood swings or depression
The complexity of PCOS symptoms can make it challenging to manage, but with the right approach, these symptoms can be alleviated.
The Importance of Diet in PCOS

Diet plays a critical role in managing PCOS symptoms and can even serve as a non-pharmacological treatment for some women. Since PCOS is closely tied to insulin resistance, a diet that controls blood sugar levels can help regulate insulin production and reduce the risk of related conditions, such as type 2 diabetes. Furthermore, a healthy diet can help regulate weight, which is vital for managing PCOS, as weight loss can improve menstrual regularity and boost fertility.
A well-balanced diet can also reduce inflammation and control hormonal imbalances, both of which are common in women with PCOS. Since no one-size-fits-all solution exists, it’s essential to understand which foods to include in a PCOS treatment diet and which to avoid.
Foods to Eat for PCOS Treatment
Incorporating nutrient-dense foods into a PCOS treatment diet is essential for managing symptoms and promoting hormonal balance. Below are some of the best foods to include in your diet if you have PCOS:
1. High-Fiber Foods
Foods rich in fiber can help combat insulin resistance by slowing down digestion and reducing the impact of sugar on the blood. Fiber also aids in maintaining a healthy gut, which can contribute to better overall health and digestion.
- Whole grains like oats, quinoa, and brown rice
- Legumes such as beans, lentils, and chickpeas
- Vegetables like broccoli, cauliflower, leafy greens, and carrots
- Fruits such as berries, apples, and pears
2. Lean Protein Sources
Protein is vital for balancing blood sugar levels and reducing cravings, which is crucial for those with insulin resistance. Opting for lean protein sources can also support weight management without contributing to excess fat intake.
- Poultry such as chicken and turkey
- Fish, especially fatty fish like salmon, sardines, and mackerel (rich in omega-3s)
- Plant-based proteins like tofu, tempeh, and legumes
- Eggs, especially free-range and organic varieties
3. Healthy Fats
Healthy fats are essential for hormone production and regulation, making them a critical part of a PCOS treatment diet. Omega-3 fatty acids, in particular, have been shown to reduce inflammation and improve symptoms associated with PCOS.
- Avocados
- Nuts and seeds (like almonds, chia seeds, flaxseeds, and walnuts)
- Olive oil and coconut oil
- Fatty fish (as mentioned above)
4. Low Glycemic Index (GI) Foods
Low-GI foods release sugar slowly into the bloodstream, helping to manage insulin levels and reducing spikes in blood sugar. For women with PCOS, this is essential for keeping insulin resistance at bay.
- Non-starchy vegetables such as leafy greens, cucumbers, and bell peppers
- Whole grains like quinoa, oats, and barley
- Most fruits, particularly berries, apples, and pears
- Legumes like beans, chickpeas, and lentils
5. Anti-Inflammatory Foods
PCOS is often linked to chronic inflammation, which can exacerbate symptoms like fatigue, weight gain, and insulin resistance. Including anti-inflammatory foods in the diet can help reduce these symptoms and improve overall health.
- Turmeric
- Ginger
- Green leafy vegetables
- Berries
- Olive oil
- Fatty fish high in omega-3s
Foods to Avoid for PCOS Treatment

Just as some foods can help manage PCOS symptoms, others can make them worse. Avoiding foods that contribute to insulin resistance, inflammation, and hormonal imbalances is key to a successful PCOS treatment diet. Here are some foods to limit or avoid:
1. Refined Carbohydrates
Refined carbs can cause spikes in blood sugar levels, exacerbating insulin resistance. These types of carbs are quickly broken down into sugar in the bloodstream, leading to hormonal imbalances.
- White bread, pasta, and rice
- Pastries, cookies, and other baked goods made with white flour
- Sugary cereals
- Snack foods like crackers and chips
2. Sugary Foods and Beverages
Sugar-laden foods and drinks can lead to insulin spikes, inflammation, and weight gain, all of which worsen PCOS symptoms.
- Sugary sodas and energy drinks
- Candy, chocolate, and other sweets
- Fruit juices (unless unsweetened or homemade with no added sugars)
- Sugary breakfast items like donuts and pastries
3. Processed and Fast Foods
Processed and fast foods often contain unhealthy fats, refined carbs, and artificial additives that can increase inflammation and worsen PCOS symptoms.
- Packaged snacks like chips, cookies, and crackers
- Frozen meals, especially those high in sodium and unhealthy fats
- Fast food items such as burgers, fries, and pizza
- Foods high in trans fats like margarine and some store-bought baked goods
4. Dairy Products
While not all women with PCOS need to avoid dairy, some studies suggest that dairy can increase insulin levels and contribute to hormonal imbalances. For women sensitive to dairy, cutting back on or eliminating milk, cheese, and yogurt may improve symptoms.
- Full-fat milk and cream
- Cheese
- Ice cream and other dairy-based desserts
5. Alcohol
Alcohol can interfere with blood sugar regulation and may exacerbate hormonal imbalances in women with PCOS. It’s best to limit alcohol intake or avoid it altogether if you are trying to manage PCOS symptoms.
- Beer and sugary cocktails
- Wine and spirits with mixers high in sugar
The Role of Weight Management in PCOS Treatment
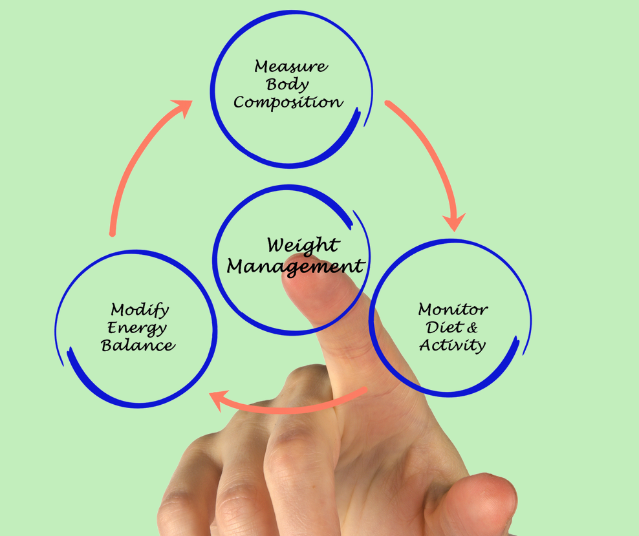
Weight management is a critical aspect of PCOS treatment, as excess weight can worsen insulin resistance and hormonal imbalances. Studies have shown that losing even 5-10% of body weight can significantly improve symptoms such as irregular periods, acne, and hirsutism, and can also enhance fertility in women struggling to conceive.
A PCOS treatment diet that focuses on nutrient-dense, whole foods can help with weight management. In addition to dietary changes, regular exercise is essential for improving insulin sensitivity, promoting weight loss, and managing stress levels—another factor that can affect PCOS symptoms.
PCOS and Fertility Treatment
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal disorders among women of reproductive age, affecting an estimated 1 in 10 women worldwide. One of the most challenging aspects of PCOS for many women is its impact on fertility. The condition can interfere with ovulation, making it harder to conceive. However, with the right PCOS treatment, many women with this condition can successfully manage their symptoms and improve their chances of getting pregnant.
How PCOS Affects Fertility
In women with PCOS, the ovaries may produce an excessive amount of androgens (male hormones), leading to irregular ovulation or anovulation (lack of ovulation). This can make it difficult for a woman to conceive since regular ovulation is necessary for fertilization to occur. Women with PCOS may also have polycystic ovaries, which are enlarged ovaries with numerous small cysts, further complicating the process of releasing eggs.
In addition to ovulation problems, PCOS can also lead to other issues that impact fertility, such as insulin resistance, obesity, and hormonal imbalances. Insulin resistance, which is common in women with PCOS, can increase the production of insulin, which in turn may affect hormone levels and further disrupt ovulation.
PCOS Treatment Options for Improving Fertility
The good news is that PCOS treatment options can help regulate ovulation, balance hormones, and improve the chances of conception. The treatment plan varies based on the severity of symptoms, the woman’s age, and her fertility goals. Below are some of the most effective PCOS treatment options for women struggling with fertility issues:
1. Lifestyle Modifications
For women with PCOS, lifestyle changes can play a crucial role in improving fertility. Maintaining a healthy weight, adopting a balanced diet, and engaging in regular physical activity can help manage insulin resistance and reduce the impact of PCOS on fertility. Even modest weight loss (5-10% of body weight) can improve hormonal balance, promote regular ovulation, and increase the chances of conception.
2. Medications to Induce Ovulation
One of the primary treatments for PCOS-related infertility is medication that stimulates ovulation. These medications help regulate the menstrual cycle and encourage the release of eggs from the ovaries.
-
Clomiphene Citrate (Clomid): Clomid is often the first-line treatment for inducing ovulation in women with PCOS. This oral medication works by stimulating the ovaries to release eggs. It’s effective in about 80% of women with PCOS and leads to ovulation in approximately 60-70% of those women.
-
Letrozole (Femara): Letrozole is another oral medication used to stimulate ovulation. It’s often preferred over Clomid because it has been shown to be more effective in some women with PCOS and may have a lower risk of multiple pregnancies.
-
Gonadotropins: If Clomid or Letrozole does not work, a more potent option is injectable gonadotropins, such as FSH (follicle-stimulating hormone) and LH (luteinizing hormone). These medications stimulate the ovaries directly and are often used in conjunction with ultrasound monitoring to prevent ovarian hyperstimulation syndrome (OHSS) and multiple pregnancies.
3. Insulin-Sensitizing Medications
As insulin resistance is common in women with PCOS, medications that improve the body’s response to insulin can help regulate hormones and improve fertility. Metformin, a medication commonly used to manage type 2 diabetes, is often prescribed to women with PCOS to help lower insulin levels and promote ovulation. Metformin can also aid in weight management and reduce the risk of gestational diabetes in pregnant women with PCOS.
4. Surgical Options: Ovarian Drilling
If medications alone do not help induce ovulation, a surgical procedure known as ovarian drilling may be recommended. This minimally invasive surgery involves making small incisions in the ovaries and using a laser or electrical current to destroy small parts of the ovarian tissue. This can reduce the production of androgens and help restore regular ovulation in women with PCOS. Ovarian drilling is usually recommended when other fertility treatments have failed.
5. Assisted Reproductive Technologies (ART)
For women who do not respond to medications or have more complex fertility issues, assisted reproductive technologies like in vitro fertilization (IVF) may be an option. IVF involves retrieving eggs from the ovaries, fertilizing them in the lab with sperm, and then transferring the resulting embryos into the uterus. IVF can be highly effective for women with PCOS, particularly those with severe ovulatory dysfunction or other fertility issues.
Managing PCOS Beyond Fertility
While the focus of treatment for many women with PCOS may be fertility, it’s also essential to address the broader aspects of the condition. Managing symptoms such as acne, excessive hair growth (hirsutism), and irregular periods can improve overall well-being. Additionally, treating insulin resistance and maintaining a healthy weight can help prevent long-term complications like type 2 diabetes and heart disease.
Conclusion: The Power of Diet in PCOS Treatment
When managing PCOS treatment, diet plays a crucial role in improving symptoms, restoring hormonal balance, and enhancing fertility. While there is no one-size-fits-all diet for women with PCOS, evidence suggests that a well-balanced, nutrient-dense approach can significantly help control many of the condition’s symptoms, including insulin resistance, irregular periods, and weight management issues.
The Role of Diet in PCOS Treatment
For women with PCOS, the focus of PCOS treatment often revolves around addressing hormonal imbalances and managing the various metabolic issues associated with the condition. One of the most common challenges faced by women with PCOS is insulin resistance, where the body’s cells do not respond properly to insulin, leading to higher insulin levels.
This can contribute to weight gain, irregular periods, and an increase in androgens (male hormones), which can worsen symptoms like acne, hair thinning, and excessive hair growth. A carefully planned diet can help combat insulin resistance, regulate hormone levels, and reduce the risk of long-term health complications like type 2 diabetes.
Key Dietary Changes for Effective PCOS Treatment
1. Low Glycemic Index (GI) Diet
A low-GI diet is one of the most recommended dietary strategies for managing PCOS treatment. Foods with a low glycemic index are digested more slowly, leading to gradual increases in blood sugar and insulin levels. By stabilizing insulin levels, a low-GI diet can reduce the risk of developing insulin resistance and support more regular ovulation.
- Examples of low-GI foods include whole grains (like quinoa and oats), legumes (lentils, chickpeas), non-starchy vegetables (spinach, kale), and fruits (berries, apples, and pears). These foods help maintain steady blood sugar levels, reduce inflammation, and support overall hormonal balance.
2. Incorporating Healthy Fats
Incorporating healthy fats into the diet is another key strategy in PCOS treatment. Healthy fats can improve insulin sensitivity, reduce inflammation, and support hormone production. Essential fatty acids, particularly omega-3 fatty acids, have been shown to have a positive effect on both insulin resistance and androgen levels.
- Sources of healthy fats include fatty fish (salmon, mackerel), chia seeds, flaxseeds, walnuts, and avocado. These fats also have anti-inflammatory properties, which can be beneficial for managing symptoms like acne and hair loss, common in women with PCOS.
3. Increased Fiber Intake
Dietary fiber is essential in a PCOS treatment plan because it helps to regulate blood sugar levels, promote healthy digestion, and support weight management. A high-fiber diet can also help reduce the impact of insulin resistance by slowing the absorption of sugars and improving insulin sensitivity.
- High-fiber foods include vegetables, fruits, legumes, whole grains, and nuts. These foods not only support hormonal balance but can also aid in weight loss, which is particularly important for women with PCOS who may struggle with weight management.
4. Protein-Rich Foods
In women with PCOS, protein plays an important role in managing insulin resistance and promoting satiety, which can help prevent overeating and support weight loss. Including lean proteins in meals and snacks can help keep blood sugar levels stable throughout the day.
- Protein-rich foods include chicken, turkey, tofu, beans, lentils, and eggs. These help regulate appetite, curb cravings, and provide the building blocks for healthy hormone production.
5. Anti-Inflammatory Foods
Chronic inflammation is often associated with PCOS, and incorporating anti-inflammatory foods into the diet can help mitigate this. Inflammation can exacerbate insulin resistance, hormone imbalances, and other symptoms of PCOS. A diet rich in antioxidants and anti-inflammatory nutrients can help lower inflammation levels and support overall health.
- Anti-inflammatory foods include foods rich in antioxidants, like berries, leafy greens, tomatoes, and cruciferous vegetables (such as broccoli and cauliflower), as well as spices like turmeric and ginger. These foods help calm the body’s inflammatory response and support the healing process.
Specific Diet Plans for PCOS Treatment
Several popular dietary approaches have been shown to be beneficial for women with PCOS. While the optimal diet can vary depending on the individual’s needs, preferences, and specific symptoms, the following plans have been highlighted in research as beneficial for PCOS treatment:
-
The Mediterranean Diet: Rich in fruits, vegetables, whole grains, lean proteins, and healthy fats (especially olive oil and nuts), the Mediterranean diet is known for its anti-inflammatory properties and positive effects on insulin sensitivity. This diet may also support heart health, which is crucial for women with PCOS Treatment, as they are at a higher risk for cardiovascular issues.
-
The DASH Diet (Dietary Approaches to Stop Hypertension): Originally designed to reduce high blood pressure, the DASH diet is high in fiber, low in sodium, and emphasizes healthy fats, fruits, and vegetables. It can be effective in managing insulin levels and promoting weight loss.
-
The Low-Carb or Ketogenic Diet: Some women with PCOS Treatment find success with low-carb or ketogenic diets, which reduce carbohydrate intake to lower insulin levels and support fat burning. While these diets are not for everyone, they have been shown to improve insulin sensitivity and promote weight loss in some individuals.
The Importance of Individualized PCOS Treatment
While diet is a critical component of managing PCOS, it’s important to note that PCOS treatment should be individualized. Every woman’s experience with PCOS is unique, and dietary needs can vary depending on factors like age, lifestyle, severity of symptoms, and the presence of other health conditions (such as obesity, type 2 diabetes, or hypertension).
It’s highly recommended that women with PCOS work with a registered dietitian or healthcare provider to develop a tailored meal plan that fits their specific needs and supports their long-term health goals.
The Role of Supplements in PCOS Treatment
In addition to a balanced diet, certain supplements can support women with PCOS by addressing nutritional deficiencies and promoting hormonal balance. For instance, Inositol (a type of sugar related to the B-vitamin family) has been shown to improve insulin sensitivity and promote regular ovulation in women with PCOS.
Another commonly recommended supplement is Omega-3 fatty acids, which help reduce inflammation, balance hormone levels, and improve overall metabolic health. Vitamin D deficiency is also prevalent in women with PCOS, and ensuring adequate levels can support insulin regulation, weight management, and even fertility.
Supplements, while helpful, should be taken under the guidance of a healthcare provider, as overuse or improper supplementation may lead to adverse effects. Additionally, while supplements can support a PCOS treatment plan, they are not a substitute for a nutritious diet and should always be viewed as complementary to healthy eating and lifestyle habits.
The Importance of Exercise in PCOS Management
While diet is a cornerstone of PCOS treatment, regular physical activity plays a critical role in improving symptoms, particularly in relation to insulin resistance and weight management.
Exercise helps the body use insulin more effectively, lowers blood sugar levels, and encourages weight loss—key components in managing PCOS symptoms. Cardiovascular exercises, such as walking, swimming, or cycling, can improve heart health and help with weight control.
Additionally, resistance training or strength-building exercises can improve muscle mass, enhance metabolism, and support hormonal balance.
For women with PCOS Treatment, finding a sustainable and enjoyable exercise routine is vital for long-term management. Engaging in at least 150 minutes of moderate exercise per week, as recommended by health guidelines, can significantly improve both physical and mental well-being.
Read more :Polycystic ovary syndrome
Managing Stress and Mental Health in PCOS
PCOS Treatment can take a toll on mental health, contributing to increased anxiety, depression, and stress. These emotional challenges can, in turn, worsen physical symptoms, creating a vicious cycle. Stress management is essential for improving the quality of life for women with PCOS Treatment.
Activities such as yoga, meditation, deep breathing exercises, and mindfulness practices can help reduce stress levels and improve mood. Research has shown that yoga, in particular, can positively impact insulin sensitivity, reduce androgen levels, and improve overall well-being in women with PCOS.
Therapy and support groups can also provide emotional relief for women struggling with the mental health impacts of PCOS. Addressing the psychological aspects of PCOS is just as crucial as managing physical symptoms, as mental health is deeply interconnected with overall hormonal balance and well-being.